ALZHEIMER'S disease is not something we usually think about if we don't have to. For me, it all started when my father, at age 70, began seeing visions. Now everyone knows you're not supposed to see things that aren't there, but my dad, ever an imaginative guy, began seeing strange people in his bedroom. The first was a very tall Indian man wearing a blue turban who gazed at my father peacefully for a while and then faded away. My father also saw beautiful patterns on walls and ceilings that would move and alter as he looked at them. Around this time, my father's memory lapses became more severe.
As with most families, we didn't want it to be Alzheimer's and, as luck would have it, there's no conclusive test for the disease, so we still don't know. Dad also had severe Lyme disease just before the visions started and his memory got worse. Maybe it's a Lyme-related disorder, also known to cause neurological problems? Maybe it's another kind of dementia altogether? Maybe it's just old age?
Whatever it is, it got my attention. Realizing that knowledge is power, I decided to learn a bit more -- perhaps an understatement since I knew next to nothing about dementia before this. What I learned was both depressing and encouraging. On one hand, there's modern science with its black-and-white discussion of symptoms, treatments, disease progression, and outcomes. Then there are the caregiver stories, which are by turns uplifting and hair-raising. What's missing is a sense of the patients themselves and what they're going through inside.
With my father's health problems, I've felt that there was another dimension to his decline, a spiritual and maybe even metaphysical element, that's especially noticeable in a disease like dementia, where such core concepts as memory, selfhood, reality, and death are so openly intertwined. So while I researched the nuts and bolts of Alzheimer's and dementia, elder care in America, side effects of neuroleptic drugs, and the problems of caregiving, I was also alert to evidence that there is more to such disorders than the misfiring of dying neurons. And evidence of that I did find. But we'll start with the medical perspective.
A Grim Corridor: The Medical View of Alzheimer's
Alzheimer's disease is the most common of several varieties of dementia, of which the dominant feature is severe short-term memory loss. It was first 'discovered' or identified April 8, 1906 when a Dr. Alzheimer in Frankfurt, Germany lost a female patient named Auguste D. to the disease. On examining her brain, Dr. Alzheimer discovered the now tell-tale plaque of tangled neurons that is the hallmark of the disease. Dementia in old people was already part of the medical canon, with the name "senile dementia." But Auguste was only 51 when she began showing symptoms. Hence, Alzheimer's disease was thought to be something different than simple senility.
Nowadays, all psychotic symptoms in the elderly are classed as dementia, usually under the catch-all term Alzheimer's disease. However, there are still some in the medical profession who use the term Alzheimer's disease only when it strikes younger people and dementia when it affects people over 65. I use the terms interchangeably in this article.
Symptoms of Alzheimer's and most forms of dementia include the aforementioned memory loss, as well as excessive emotionalism and moodiness, loss of inhibition, disorientation, personality changes, visual and auditory hallucinations, extreme restlessness, repetitive talking or actions, depression, losing track of time, and getting lost.
Other symptoms can include wandering and sundowning, the latter a common problem for old people in which confusion and psychotic symptoms get worse at night. Symptoms of late stage Alzheimer's are more serious and include loss of the ability to use language, perform routine tasks such as bathing or getting dressed, recognize bodily cues (leading to incontinence), or even swallow food. In other words, there may come a time when the patient can no longer speak, feed, or clothe himself, and requires constant care.
Alzheimer's can affect people as young as 40, but is more common in people over 65 where the chances of developing the disease increase incrementally with age. In people 65 years old, there is a 1 percent chance of Alzheimer's, while in people over 85, the prevalence is approximately 50 percent. So Alzheimer's is common in the elderly. And while it is considered 'terminal', it is not a disease that kills you outright. Most Alzheimer's patients die of secondary infections such as pneumonia or sepsis brought on by inactivity in late stages of the disease. (1)
There is no known cause or trigger for Alzheimer's. What is known is that it kills brain cells, and that the process begins long before the person begins to exhibit symptoms. Scientists speculate that amyloid plaques -- clusters of proteins outside of nerve cells -- and tangles -- twisted strands of a different protein that form inside nerve cells -- are to blame for the degeneration caused by Alzheimer's. However, autopsies of people who did not have Alzheimer's have revealed plaque formation as well. The damage to proteins in Alzheimer's is an example of a protein-folding disorder, putting it in the same class as other neurodegenerative protein-folding diseases, including Parkinson's, Huntington's, ALS (Amyotrophic Lateral Sclerosis, aka Lou Gehrig's Disease), and ominously, CJD (Creutzfeldt Jakob Disease: the human form of Mad Cow). (2)
Alzheimer's and dementia cannot really be treated, as there is no known drug that reverses the disease once it starts. There are drugs that claim to slow the progression of the disease for some, and there are tranquilizers and antipsychotics that can reduce some of the more troublesome symptoms such as hallucinations or screaming outbursts. But many of the drugs don't work and some (including drugs prescribed for other ailments such as high blood pressure) can make the dementia worse. (3)

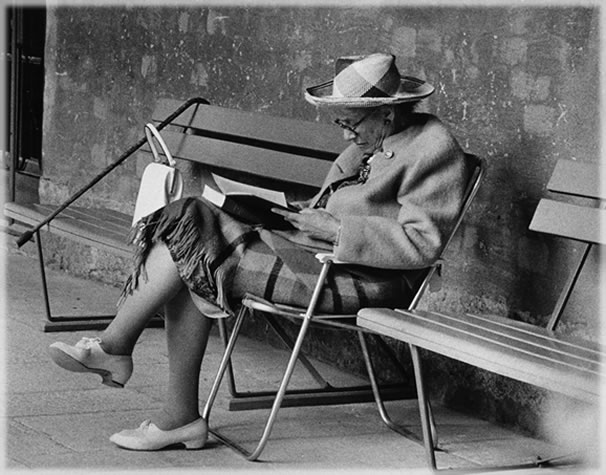
Still frame from the 1955 movie, Dementia, courtesy of Cine-Studies.net
Medicating Dementia
Dementia is a medical term for psychosis, but its literal meaning is to be 'out of one's mind'. One of the reasons they call it dementia is that in addition to memory loss, psychotic behavior is common.
Psychotic symptoms fall into two categories: delusions and hallucinations. Anyone who's spent time with the very old knows that it's not uncommon for an old person to get it in their head that someone is out to get them and to be excessively worried. In psychiatric terms, this person is exhibiting paranoia -- irrational fear. Common delusions of people with dementia include the belief that a stranger is in the house, that someone is trying to steal from them, that someone (often a family member) is trying to kill them, or that their spouse has been unfaithful.
Hallucinations also occur frequently, both auditory and visual, although visuals are more common. Approximately 40-60 percent of Alzheimer's/dementia patients hallucinate. Often a patient will start out with auditory hallucinations -- one woman constantly heard The Star Spangled Banner before moving on to visual hallucinations. The types of hallucinations people have are quite varied, but there are common threads. Patients frequently report seeing dead relatives or pets, imposing strangers in strange garb, religious figures, intruders, strange animals, and even angels. Some Alzheimer's patients get very rattled during these episodes. Others, and this has been much more the case in the stories reported to me, are matter-of-fact about their unusual experiences and merely want to tell someone about them.
Nevertheless, hallucinations are troubling to caregivers, especially when they cause fear in the patient, and psychotropic drugs called antipsychotics and neuroleptics are often prescribed to control both delusions and hallucinations. Until the mid-1990s, when federal regulations went into effect prohibiting excessive use of neuroleptic drugs as chemical restraints, nursing homes routinely prescribed these drugs to control patient's hallucinations as well as non-psychotic behavioral issues such as public masturbation, screaming, being disruptive to other residents, and wandering. Even today, these types of drugs are frequently prescribed. This might be okay if a) the drugs worked and b) they did not have a long list of serious side effects.
There are two classes of drugs used to control hallucinations and behavior in dementia patients. The first, called 'typical' drugs, are the older class which includes Haldol, Navane, Prolixin and Mellaril. These drugs work by blocking dopamine receptors in the brain (also called dopamine inhibitors). There is a newer, so-called 'atypical' class of antipsychotic drugs which affect multiple neurotransmitter systems and include Respiridol and Seroquel. The newer antipsychotics are reported to cause fewer side effects but are still serious pharmaceuticals. (4)
The most common side effects of these drugs (both classes) are tardive dyskinesia ("unwanted movements of the lips, face, hands, arms, and feet as well as rocking of the pelvis and jerking motions of the diaphragm"), drug-induced parkinsonianism (stiffness, shuffling gait), akathisia (extreme restlessness and agitation) or a combination of the three. Thirty to 50 percent of patients on antipsychotic medication will manifest some combination of these symptoms in time. (5)
But these symptoms only include those that affect the motor system. Antipsychotic drugs can also, in rare cases, destroy the autonomic nervous system resulting in severe illness and death. Or they can produce effects such as sedation, apathy, and confusion (this in people who are already confused). There can be gait abnormalities leading to falls (this in people who are already unsteady on their feet). And of course: "All antipsychotic medications can produce medical complications including: 1) glucose and lipid intolerance, 2) cardiac conduction problems, 3) bone marrow alterations, and 4) alteration of metabolism of other medications." (6)
As you might imagine, there are now strict government controls over how these drugs may be prescribed, for what conditions, for how long, and at what dosages. Nursing homes are required to evaluate and potentially lower dosages every six months for patients on one or more neuroleptic drugs. This is good news. A recent study published in the Journal of the American Medical Association suggests that antipsychotic drugs result in a higher death rate for those who take them. (7) But although the drugs are not recommended for long-term use, many patients stay on them for years and nursing homes still routinely prescribe them as a method of curtailing annoying behaviors in residents.
As for the effectiveness of antipsychotic drugs, the jury is out. Most traditional medical sources, such as the Alzheimer's Foundation, say that neuroleptic drugs can greatly improve the patient's quality of life if the drugs are carefully prescribed and monitored. (8) Family caregivers, however, cite many examples in which the drugs have been more problematic than helpful. In some cases, antipsychotics simply don't help the hallucination problem; in other cases, they cause new problems or bring on serious side effects. Some examples of problems include exacerbating sundowning (resulting in the patient being up all night) and causing excessive 'dopiness' in the patient (a side effect known as sedation). (9, 10, 11)
While many Alzheimer's patients will do a stint on antipsychotics as a result of one or another behavior problem, there is medical and anecdotal evidence that in some cases, the meds only make the dementia worse. Here's one striking example from the son of an Alzheimer's patient:
"My father has had the dementia for over 12 years now. He would have died many years ago, I believe, except for the action I took of removing him from the medications that the doctors had prescribed for him. When I began caring for him seven years ago, they prescribed Prozac, Buspar and halioperiodal (Haldol) to help control him. For two years he was on these meds and progressively grew worse, to the point of loss of balance, loss of speech, incontinence, the whole nine yards. In about 1996, I became aware of the uselessness of these drugs and removed him from those meds and quit taking him to the doctors. Needless to say, he improved dramatically, regained his balance, diet, continence, speech and strength." (12)
Although it's hard to find anyone who'll say this, it does seem that there is a tendency to medicate the elderly for the convenience of (younger) caregivers who often find the behavior of demented elders annoying and their visions disturbing. And while some dementia patients are truly disturbed -- up all night talking to invisible people, yelling, and making a ruckus -- not all hallucinating old folks are that problematic. (13)
What's So Bad About Seeing Dead Relatives?
In general, we tend to regard hallucinations and other manifestations of mental disorder as abnormal and 'bad'. But we might ask, are they really? In order to fairly evaluate the hallucinatory experiences of the elderly, it's helpful to know what they are. Here are a few examples of what seem to be fairly common hallucination stories, with or without a diagnosis of dementia:
"My mom is a very active 80-year-old who still works full time in an office environment. As a matter of fact, she just received a promotion. She's had a few disturbing nights. She dreams that a tall woman, in a long dress, is standing at the foot of her bed talking to her and trying to wake her up. Mom says that she wakes up and the woman is still standing right there. My mother lives alone. She said the first three or four times this happened she screamed. That's around the time she told me about it. There have been other times, in these past few years, when she'd wake up and see my deceased father sitting on his side of the bed. She doesn't seem bothered when she sees my dad, but the woman at the foot of the bed scares her, even though she's not doing anything menacing."
-- Planet Waves reader
"Over the past nine months or so, she has reported increasing incidence of hallucinatory episodes. At first, she tended to hear music (opera usually) late at night. Then she started reporting seeing her sister (who passed two years ago) walking in the house late at night). Next, she heard people working on the house during the day -- no one was working on the house. More recently, she has made supper for my father (who passed 12 years ago) and made lunch for people she thought were working on the house." (14)
- Alzheimer's Forum
"My father had emphysema and dementia (at least according to the doctors). He was born in South Dakota, USA. He died four years ago on May 18th. One evening he was sitting on his couch reading, and glanced down his hallway. He saw his grandmother in the hallway, she turned, smiled and waved at him and continued on. He used to wake up in the morning thinking our dog (from childhood days, gone over 30 years) was lying beside him, asleep. And he would wake up petting the dog. And then he said he woke up in the middle of the night, and my mother was sleeping beside him. He asked her if it was time for him to leave with her, and she told him -- not yet, but she would be with him until the end. For the last month of his life, he said he woke up in the morning with mom at his side, and believed she had snuck out to make him his favorite breakfast. And the last day of his life he said mom had run out to get things ready, but he would like us to chat with his old army buddies while she was gone. My sister and I swear we saw about ten men dressed in Second World War uniforms around our dad. Some very young, and some very old, very indistinct -- like a dream as you are waking up. Then he died that night. And strangely enough, his second wife buried him in a military cemetery, not in the local cemetery."
-- Planet Waves reader
There are numerous stories of this type, where the common thread is that people suddenly start to see family members who have died. Now why would this be? While science has no interest in the content of patients' visions, a little common sense suggests that perhaps because elderly people are a bit closer than the rest of us to death, 'the other side' if you will, they have insights the rest of us lack. And if you have any belief in an afterlife, it's not that much of a stretch to think that as we get older and closer to dying, our deceased relatives might take an interest in helping us across.
As it turns out, there is evidence to support this idea, as another group of people who hallucinate wildly are those close to death. One article reports the results of a four-year study by physicians Karlis Osis and Erlendur Haraldsson of over 50,000 dying patients in the U.S. and India: "In both cultures, patients commonly reported deathbed visions of movement toward something and of being greeted by deceased loved ones who were helping them to 'cross over' in their last moments." (15)
There are other similarities. Journeying, traveling and 'going home' are common themes in the hallucinations of the dying. As one hospice nurse put it: "The dying recognize 'that they're going from one world to another one' or the feeling that they're 'going somewhere.'" (16)
In the case of dementia patients, going home is a theme as well. According to the Mayo Clinic: "The desire to 'go home' is common in people with Alzheimer's disease -- even when they're in the home where they've lived independently for years." The article goes on to ascribe this phenomenon to patients who are 'living in the past'. (17) Not everyone wants to go home though. The caregiver quoted above, whose father improved after being taken off medication, reports the following:
"My dad cannot speak clearly while awake, but when sleeping he is very clear, speaking with invisible entities. On more than five occasions, he has gotten into arguments with those entities, yelling at them saying, 'No, I won't go with you. I won't go with you. Go away'. And other statements in that regard. Once he even mentioned that he did not want to go to the light!" (18)
I have a similar story regarding my own 99-year-old grandmother, who is generally lucid by my standards, but has had serious memory problems and on-and-off hallucinations for the last five years. She too argued with invisible entities in the night, and toward the end of the time she lived in her own house, she would talk frequently about 'going home'. We became convinced that she wanted to go home to her family -- all 11 of whom had died by then. Later that year however, after finally allowing herself to be put into a nursing home, she reported to my aunt that she'd had a dream in which she went to a big house where all her dead sisters and brothers were waiting for her. Her oldest sister came forward and said to her, "Come be with us." According to my grandmother, when she heard that, she said "no" and walked right out of there.
I've also run across two reports of unusual psychic ability in Alzheimer's patients. One friend told me that while she was taking care of an elderly woman with Alzheimer's, she got really impatient and angry with her (not uncommon for caregivers) and thought murderous thoughts. The old lady turned to her and said "You're not going to kill me!" Needless to say, my friend was more careful after that.
Another caregiver relates this story:
"I took care of my mother, with Alzheimer's, until she died a few years ago. One of the hard aspects of doing this was that I had to keep my mind as BLANK as possible while in her surroundings, or else she would pick up on my thoughts and keep 'nagging' me all day. If I would only think something like 'I need to make a dentist appointment today', she would keep reminding me all day long ('Have you called the dentist yet?' many, many. many times over and over...).
"She could get upset about things she had NO WAY of knowing. For example, there was the incident of the cat. At a certain moment I found a tiny little kitten and took care of it until I had found a home for it. My mother, not much of a cat lover, got very upset about the cat in my house (not that she had been there, or had even seen the cat) and only came by my house, a few hours after the cat was gone, and mentioned how much better it was now in my house without the kitten there."
- Planet Waves reader
Here again, we see evidence that some people with Alzheimer's and dementia have strange powers. Not only can they see dead people and spirits, some can even read your mind! Medical science will tell you that these are merely the random emanations of a disordered brain. But I'm not so sure.
The Metaphysics of Madness
Humankind has long had a fear of madness. No one wants to be the babbling idiot, and that's pretty much how most people view those afflicted with Alzheimer's and dementia. The word 'demented' itself is an epithet. Writes one caregiver: "I am at wit's end. When she relates these [hallucinatory] experiences to me either in person or on the phone, I can feel my blood pressure and heart rate increasing." Says another: "When he matter-of-factly mentions someone being in his bathroom or seeing a fire in the closet, I get chills and my blood pressure also goes up." (19)
Most caregivers want to deny their elders' hallucinations -- after all, hallucinations aren't 'real'. Isn't it kinder to point this out? As it turns out, it isn't usually helpful to do so. Most dementia patients believe in the reality of their visions and do not want them debunked. One way to annoy a demented person, apparently, is to tell them that they're seeing things. So caregivers are advised not to argue with patients about these matters, but simply to make comforting, neutral statement such as "I don't see the angel in the dustbin, but I believe that you do."
But there's another side to the human view of craziness, summed up in the phrase 'divine madness'. Throughout human history, there have been people who claim visionary experience, a nicer name for hallucinations. Among them are the prophets who talk to God and the young girls who receive messages from the Virgin Mary. Carl Jung describes several visionary experiences in his autobiography, all of which had a profound impact on his life and work. Moreover, there are plenty of ordinary people who claim to have seen ghosts. In other words, not everyone who hallucinates is regarded as crazy. Some are seen as divinely inspired.
Why this connection between madness and the divine? I would posit that mankind has made a special point of closing the doors between dimensions such that we deny the existence of anything that doesn't fit neatly into three-dimensional reality. If you do see anything out of the ordinary, you must be crazy. But there's good crazy and bad crazy. If you come back from the desert spouting messages from God (any god will do), and you have sufficient charisma to pull it off, then you're a visionary. If you're 82 and you think you just saw your dead wife in the hallway, you're demented. But who's to say that you really didn't just see your dead wife in the hall?
Many caregivers claim that Alzheimer's isn't all bad. Some say that the personality changes were good for their ailing relative, that formerly up-tight and irascible old folks became sweet and open under the influence of Alzheimer's (although the reverse is also true). Another said that although her husband eventually lost the ability to talk to her, that the love between them never died and that they continued to have fun to the end, despite his limitations. (20)
Conclusion
Alzheimer's and dementia in the elderly are tragic only if you believe that people should live forever; currently we do not. Otherwise, some deterioration over time should be expected. People do not enjoy losing their mental faculties as a rule, but in general it's not as bad for the patient as it is for the caregivers. Children and spouses often have a very hard time watching a formerly strong and sound loved one revert to childhood and helplessness.
In childhood, we come into the world empty of earthly knowledge. Gradually, we build for ourselves an identity, created out of the experiences and memories of our ongoing lives, and it is these experiences and memories that tie us to the world. But eventually, it becomes time to leave again. Many aging adults experience a second childhood, which we now call dementia. And as the trappings of life slowly drop away with age -- memory, personality, language, even recognition of self -- the person is slowly and inexorably freed from the bonds of earthly existence. Eventually, they are delivered to a dimension beyond space and time that we, the young and vibrant, can only glimpse through the visions of madmen and, if we're lucky, our elders.
Although the following quote has nothing to do with Alzheimer's disease, it sums up for me what is perhaps the greatest lesson of this strange odyssey I find myself on:
"The Pearl of Great Price, The Holy Grail, the Vision of God, Nirvana, Valhalla, Heaven, or Salvation, call it what you will, it will not be found until the individual forgets who they are, and what they are looking for. Then they shall find it. " (21)
Afterword
There are as many different manifestations of dementia as there are patients, and I was only able to cite a few examples in this article. Some patients suffer greatly from delusions and hallucinations (as well as other symptoms) while some handle them with more aplomb. While overall, drug therapy for dementia in old folks seems dicey at best and ill-advised in some cases, there are people who claim to benefit from it –- for a while at least.
If you or a loved one is dealing with this disease, don't take my word for anything. Find out what you can and come to your own conclusions. This article is merely an effort to find a more balanced view beyond the doom and gloom of medical prognosis. And as with so many things, attitude matters. Dispelling some of the fear can only help, and in that regard, I hope this article has been helpful.
Glossary
Agitation: A common symptom in Alzheimer's and dementia patients in which the person becomes very restless or performs repetitive actions.
Antipsychotic: A class of drug prescribed to control psychotic symptoms such as hallucinations and delusions.
Caregiver: Any person, either a family member or nursing home staff member, who takes care of an ailing person. People who take care of Alzheimer's patients are almost always referred to as 'caregivers'.
Delusions: A common symptom of Alzheimer's and dementia in which the patient develops irrational fears.
Hallucinations: A common problem for aging people in which they see or hear things that aren't there.
Neuroleptics: A class of tranquilizing drugs often used synonymously with antipsychotic drugs.
Screaming: A problem that can occur in Alzheimer's patients, in which the patient yells continually. This is a bigger problem in nursing homes where patients get less personal attention, but patients living at home can also exhibit this behavior. It is generally regarded as a sign that the patient is unhappy about something or in pain but can't express it.
Sundowning: A common symptom affecting elderly people in which psychotic symptoms and disorientation become more pronounced at night.
Wandering: A phenomenon of Alzheimer's in which the patient simply takes off to parts unknown. In nursing homes, this is a major problem due to liability issues. Moreover, in facilities for the elderly, one escaped patient may allow other patients to escape as well, necessitating a full search of the facility and environs for one or more missing persons.
Sources
(1) Cause of death in Alzheimer's patients
(2) "Protein Folding and Neurodegeneration: Biophysics to the Rescue?" By David Teplow, Brigham and Women's Hospital, Boston, Massachusetts
(3) The Alzheimer's Association: Myths About Alzheimer's
(4) A Short Practical Guide to Psychotropic Medications for Dementia Patients
(5, 6) Understanding Side Effects Of Neuroleptics
(7) Antipsychotic drugs may boost death risk for Alzheimer's sufferers
(8) Alzheimer's Foundation: "Psychotic symptoms can often be reduced through the carefully supervised use of medications."
(9) Healing Well Forum -- Hallucinations and dementia
"Dad was put on Seroquel for the hallucinations but it had him up and wandering all night. So Mom halved the dosage and still no good, so she stopped it."
(10) Healing Well Forum -- Hallucinations and dementia
"[My mother] is now on Sinemet and Seroquel. She was diagnosed this time last year but we do not know how long she had it. She was first put on Mirapex which worked well for about 9 months. The meds she is taking now do not seem to help with the horrific hallucinations mostly at night...the Seroquel does not seem to help her."
(11) Aging Parents and Elder Care Support Group
"We visited her physician, and he prescribed Namenda which she has been phasing into during the past 3 weeks. She is now complaining about feeling 'out of it' for about 4 hours after taking the morning dosage. She has not reported any hallucinatory incidents -- until today."
(12) Paranormal Story Archives
(13, 14) Aging Parents and Elder Care Support Group
(15, 16) From LA Times article "Taking Life's Final Exit" by Valerie Reitman
(17) Ohio Health -- Alzheimer's Behaviors: My father wants to 'go home'
(18) Paranormal Story Archives
(19) Aging Parents and Elder Care -- hallucinations and caregivers
(20) From There's Still A Person In There by Michael Castleman, Matthew Naythons, Dolores Gallagher-Thompson: "The mass media often describe Alzheimer's disease as a 'living death'. Ann disagrees. 'As human beings, we're a great deal more than how we define ourselves. It's amazing how much you can lose of what you once considered essential to your self, and still retain your humanity. Julian can no longer take care of himself, and he's down to just a few tunes and an occasional word, yet he greets me with a warm smile and a loving hug. We take our walks. We fool around. As long as I don't expect anything from him, as long as I stay in the moment, we can have fun. It's amazing to me, impaired as he is, Julian is still with me. There's still a loving person in there.'"
(21) From The Way Of Wonder: A return to the mystery of ourselves by Jack Haas
General References
The Alzheimer's Association
Dementia Directories (Alzheimer's, Huntington's, CJD, Alcohol Dementia, etc)
Alzheimer's Directories From Alzheimer's Outreach
Sprituality and Alzheimer's
A Short Practical Guide to Psychotropic Medications for Dementia Patients
Ohio Health Alzheimer's Site: Benefits of Alzheimer's Drugs